 |
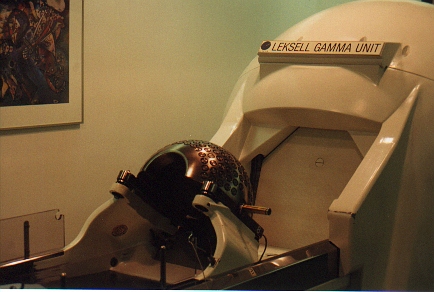
The Gamma Knife Unit |
Gamma Knife:
treating ANs with radiosurgery
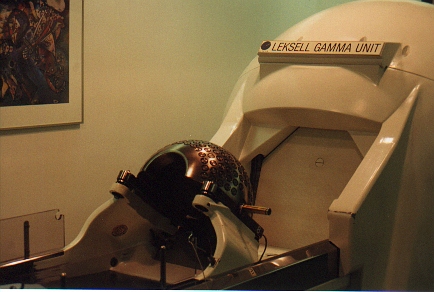 |
The Gamma Knife Unit |
1. The history of Gamma Knife radiosurgery
Gamma Knife (GK) radiosurgery has been used in AN treatment since 1968, with 6,434 AN treatments by Dec. 1996 (statistics taken from Another Perspective, a newsletter of the IRSA). Other benign brain tumors are treated with GK as well.
To learn about GKs as a treatment option, a chapter by Dr. Georg Noren of Brown/Providence Hospital in 'The Textbook of Stereotactic and Functional Neurosurgery', McGraw Hill, NY, is really worth a reading. It describes historically the evolution of the GK in the treatment of AN's over the period of the 1960's to the 90's. The title of the chapter is GAMMA KNIFE RADIOSURGERY FOR ACOUSTIC NEURINOMAS (chapter 10).
A newer, and even more encouraging report, is described in a recent issue of Another Perspective. This overview of the latest refinements and improvements in GK was written by guys from the Univ. of Pittsburgh Medical Center (Kondziolka, Lundsford, Flickinger). The section on ANs makes highly recommended reading; here is a summary. The latest report on GK outcomes for ANs comes from University of Virginia.
Pittsburgh was the first site in the US to offer GK, and has been producing impressive GK results since. Their article in the Journal of Neurosurgery ( vol 36, No. 1, January, 1995), titled Outcome Analysis of Acoustic Neuroma Management: A comparison of Microsurgery and Stereotactic Radiosurgery (authors B. Pollack, D. Lundsford, D. Kondziolka, Flickenger, et al) presented such a challenge to the medical establishment that Dr. Pollack lost his job in Pittsburgh as a result of it.
If you are interested in the history of Gamma Knife, clinical studies, and comparison of treatments for AN, we recommend the following article, which is said to be "fascinating and well written":
Gamma Surgery for Vestibular Schwannomas, by Prasad, Steiner and Steiner, published in the Journal of Neurosurgery, Vol.92, May 2000, pp.745-759.
2. What does Gamma Knife do?
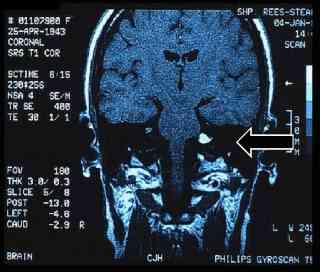
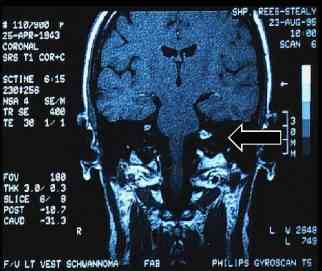
Though GK does not get rid of the tumor, it stops the tumor from growing any further, and in many cases shrinks it somewhat. The intensity of the AN contrast on the MRI is often decreased as well, indicating the death of the tumor cells. Here are typical MRI images of an AN "before" and "after" being treated by GK, kindly provided by the San Diego GK Center:
 |
 |
Acoustic Neuroma before Gamma Knife |
Acoustic Neuroma after Gamma Knife (7 month) |
As a result, Gamma Knife treatment may get rid of the symptoms that were caused by the tumor:
My "fullness" is only on the left side - the side of my AN. It is like a plugged up feeling. I had this before GK but it is getting less and less since I had GK 1 1/2 years ago.
The precision of aim during GK is assured by attaching a metal frame to the patient's head for the duration of the one-day treatment:
These are very tiny surgical screws that carry their own anesthetic. They barely penetrate, and no scar results from the small hole. The part of this procedure I hated most was getting up early in the AM and washing my hair with some special shampoo. There is no shaving involved, let me add. Some people have some bleeding when the frame is removed. I didn't. No large bandages are needed.
Given the low complication rates of GK, the biggest drawback for most patients is their fear of possible malignancy. By now, GK has been used on over 80,000 patients world wide to treat a wide variety of tumors, many demanding much higher radiation doseage than an AN. Yet, there has been no connection between GK and cancer reported in all that time. That is to say, the overall rate of brain cancer in AN patients who have been treated by GK has not been any higher than for post-surgery patients.
3. Is Gamma Knife treatment the same everywhere?
(contributed by Peter Campbell-McBride, President, Gamma Knife Surgery Support Association)
There is no such thing as a standard Treatment Plan in Gamma Knife Surgery; no-one should suggest to you that it is a "cookie-cutter" procedure. The order in which the procedure is carried out is standard, but the number of shots, the collimator size, and the dose all vary from case to case. It is up to the individual neurosurgeon and radio-oncologist to agree on the plan; the same patient presented to three different sites would most likely get three different Treatment Plans.
In some research projects, a group of sites will agree to use exactly the same dose levels on similar size lesions for comparative purposes on a known patient group, but that does not apply to routine treatments.
I don't know who said that there is a consistant protocol, but I assure you there isn't. Some sites will try to develop a plan using only one size of collimator to save time in changing helmets. Others will use a few (<5) large shots instead of smaller variable size shots to cover the lesion. In my experience the more experienced and clinically robust sites will take more time and trouble in Treatment Planning, hence I advise against using low volume inexperienced sites.
4. Other Gamma Knife resources
IRSA (international radiosurgery support organization) can answer many other questions about Gamma Knife. Many GK patients have published their stories in the AN Archive's patient directory. And here is the homepage of the Elekta, the company manufacturing Gamma Knife apparatus.
Last Edited: Wednesday, October 30, 2002